Billing Codes Demystified
By TherapyNotes, LLC on March 21, 2018

When creating insurance claims, determining what code to bill can pose a serious challenge. Often, it may be hard to even figure out where to begin when looking for your billing codes, and with so many different codes and identifiers included on claims, it can be confusing to determine what each code is for.
Where do billing codes come from?
Most of the commonly used billing codes are actually a direct product of HIPAA. The Administrative Simplification Rule requires the creation of standards for the exchange of information for healthcare claims, leading to the creation of standards such as national provider identifiers (NPIs). Other standards, such as Healthcare Common Procedural Coding System (HCPCS) codes, had been in voluntary use and became mandatory.
Describing Who, What, When, Where, Why, and How
When billing insurance, numerous codes exist to describe every aspect of the service rendered, including who provided the service, what the service was, when it occurred, where it occurred, why it was necessary, and additional details on how it was rendered. Each code connects to form a holistic picture of the service.
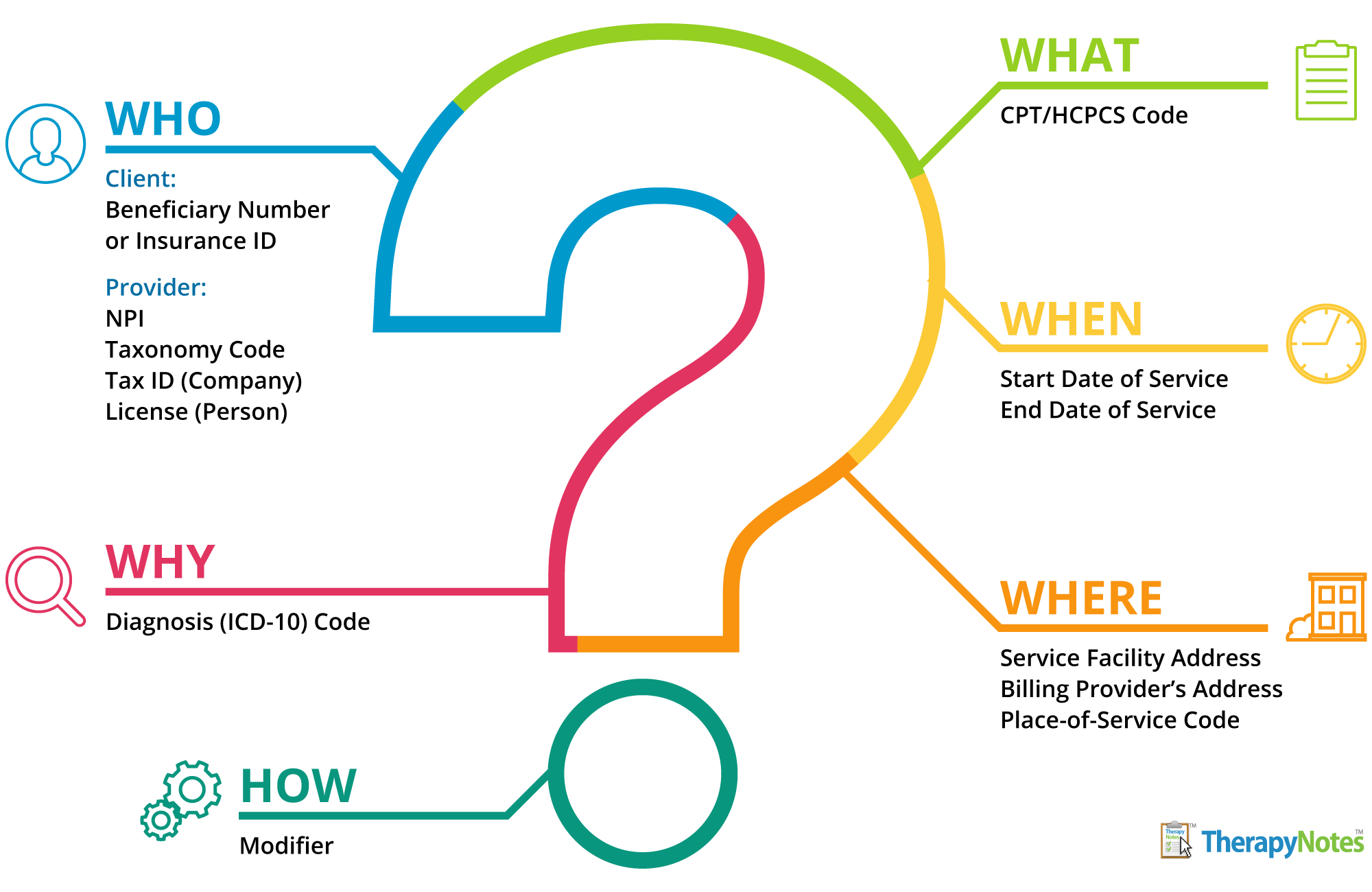
Who: Several codes are used to identify the individuals and entities involved in the claim for a rendered service. NPIs and Tax IDs identify the company and individual who rendered the service. Taxonomy codes identify these entities' specialties and scope of practice. Clients also have a beneficiary number or insurance ID number to identify them in the transaction.
What: HCPCS codes, also known as service codes, are used to describe what service was rendered and what you're billing for. HCPCS codes are broken into two levels:
- Level I: Current Procedural Terminology (CPT) codes maintained by the American Medical Association (AMA). These codes consist of five numeric characters and are used to uniformly identify medical services and procedures. CPT codes include 90834 (psychotherapy, 45 minutes with patient) and 90785 (interactive complexity). For more information, read A Quick Overview of CPT Codes on our blog.
- Level II: All other codes that could be used to identify products, supplies, and services not described through CPT codes. Level II codes are five-character, alphanumeric codes, such as H0001 - Alcohol and/or drug assessment.
There are 6,558 valid HCPCS codes, covering all levels. Each insurance company may require specific codes to represent services or restrict the use of others. To find out what codes to bill, refer to your contract with the insurance company or the billing provider’s manual if you are out-of-network.
When: Specific codes aren't used to describe when a service occurred, but date formats on claims are standardized. It is important to include both the start and end date of the service, even if that was the same date, using the MMDDYY format.
Where: The service facility address and billing provider’s address are both required on claims, and each address should include the full 9-digit ZIP code. Place-of-Service codes further describe where services are rendered. These codes identify the type of facility (such as inpatient hospital, office, telehealth, etc.) located at the address listed on the claim. Place-of-Service codes are designated by a two-digit number 01-99, such as 53 - Community Mental Health Center.
Why: Most insurances require medical necessity to pay a claim, and medical necessity is often determined by the diagnosis of an individual. The criteria for diagnosing an individual is standardized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), and the diagnosis itself is represented in a claim by a diagnosis code from the International Classification of Disease - 10th Edition (ICD-10). ICD-10 codes are typically a letter followed by a few numbers, although some codes may use a decimal and additional numbers to provide more specificity about the diagnosis. Typically, ICD-10 codes used for mental health begin with the letter F, such as F41.1 Generalized anxiety disorder.
How: The codes above provide a lot of information about services rendered. However, there may be additional information that can assist with the successful processing of a claim. This information is often contained in a modifier, a 2-character alphanumeric code that can represent a wide variety of factors that impact how a service is rendered, from the equipment used to unusual events that impacted how a service was performed. For example, the modifier AH is used to describe and bill for services provided by a clinical psychologist.
* The content of this post is intended to serve as general advice and information. It is not to be taken as legal advice and may not account for all rules and regulations in every jurisdiction. For legal advice, please contact an attorney.
Get more content like this, delivered right to your inbox. Subscribe to our newsletter.
More Content You'll Enjoy
The Best Practice Fusion Alternative for Mental Health

Supercharge your Documentation with TherapyFuel!