TherapyNotes™ 4.67 Note Template Updates
By TherapyNotes, LLC on April 9, 2021

At TherapyNotes™, we work hard to help reduce the burden of administrative tasks, allowing you to focus more of your time and effort on your clients and your business. Our copyrighted note templates have always followed the Golden Thread, automatically moving information from one note template to another to seamlessly create a holistic narrative of the client’s experience in therapy. We’ve made it easy to finish session notes in minutes, while giving you peace of mind in the event your documentation gets audited.
Now, we are proud to announce that your documentation is about to become even better. After months of research, reviewing audit templates from a wide variety of insurance companies, suggestions from our customers, and best practice guidelines from professional organizations, we’ve updated our note templates. Please read this article carefully and share with your team to ensure everyone is prepared for these upcoming changes which will be found in TherapyNotes™ 4.67, scheduled for release on April 14, 2021.
Psychotherapy Intake Notes
We’ve added new functionality to our Intake Notes to help you better capture your sessions with less effort. Intake Notes will tie directly to our upcoming Client History Form, allowing you to have your client complete the form through their portal account and then pull their responses directly into the Presenting Problem and new Biopsychosocial Assessment fields (more on these below) of your Intake Note. The new Client History Form will also be released with 4.67 with more detail provided in the release notes.
Current Mental Status
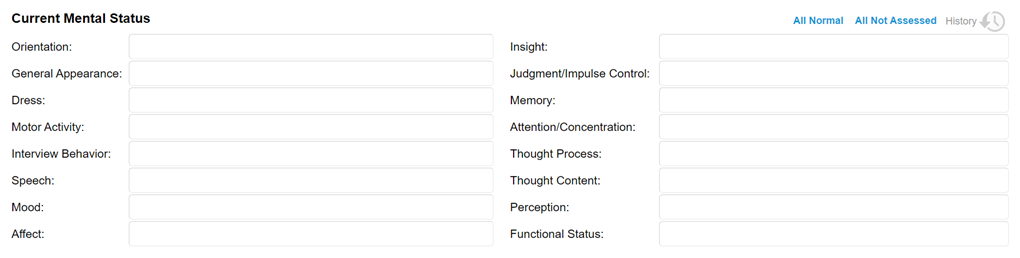
Functional Status has been added as a new option for Current Mental Status, and Judgment has been renamed "Judgment/Impulse Control." The order of items in this section has been updated for a more natural flow, and new selectable options have been added to some items. As always, we’ve kept the simple one-click option to mark all items as either within normal limits or not assessed.
Risk Assessment
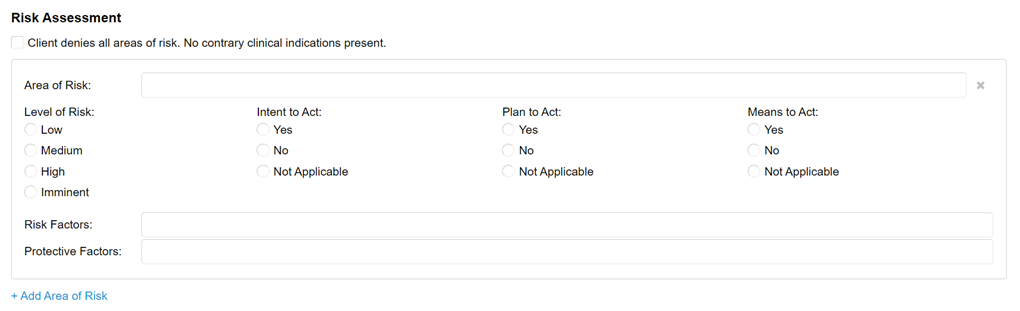
We’ve replaced the Safety Issues check boxes with a brand-new section to comprehensively assess and document risk. This section is designed to quickly capture information that follows best practices in documenting risk from both a clinical and malpractice insurance perspective.
Indicating No Risk
Instead of a blanket “None” option, a new checkbox will quickly indicate that the client denied all areas of risk. This allows for a more accurate representation of what happens in session. In addition, the checkbox captures your clinical assessment of the client denial. This shows that you did more than simply take the client at their word; you applied your clinical knowledge and skill to actually assess the client and came to the conclusion that the denial is accurate.
Area of Risk
This field will allow you to either select from a list of common areas of risk or type in a specific response. You are also able to enter any additional or more specific areas of risk for your client. You should enter only one area of risk per line, as each area can now be assessed independently. This field will be required on notes if the check box indicating the client denied all areas of risk is not selected.
Level of Risk
Just because an area of risk is present for your client does not mean it poses an immediate or grave threat. You can now indicate variance in risk over time, showing effective documentation of improvement or periods of crisis. Since each area of risk is assessed independently, you can quickly show where differences exist.
Intent, Plan, and Means to Act
Documenting these items helps justify your determination of the level of risk and shows that you completed a thorough assessment. We have included the ability to mark each item as Not Applicable, as they may not apply to some types of risk. For all areas of risk, you will be required to select one response for each of these three items.
Risk Factors/Protective Factors
These fields allow you to select multiple items from a list of common factors shown to increase or decrease the level of risk. Choose as many as apply to each area of risk or add your own items specific to your client.
+ Add Area of Risk
Click this link to add another group of fields to assess an additional area of risk. When documenting multiple areas of risk, you will be able to reorder the groups or delete an entire group at once.
Biopsychosocial Assessment
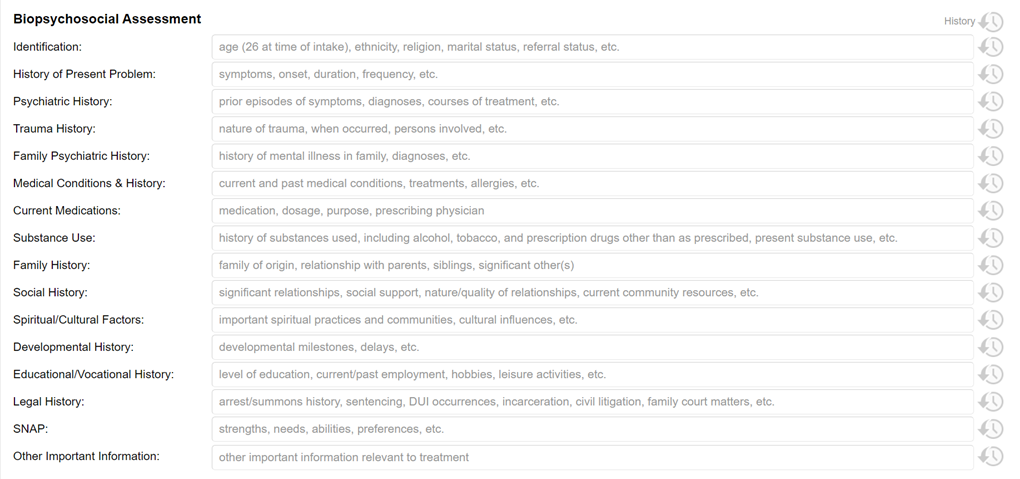
We have renamed the Background Information section to Biopsychosocial Assessment to describe your clinical role in the process more accurately—not just a history-taker but a holistic, active assessor of your client.
We updated some of the field labels and prompts to provide a more thorough review of your client and to comply with third-party requirements, including changing the Strengths/Limitations field to SNAP: strengths, needs, abilities, and preferences. Not only is this in line with CARF® documentation requirements, but it helps to take a holistic view of the personal characteristics that can help your clients succeed in treatment. We also added a new field to assess Spiritual and Cultural Factors, recognizing the significant impact these domains may have on your clients’ functioning. Every field in the Biopsychosocial Assessment continues to be optional.
Each field from History of Present Problem through Other Important Information may be populated with your client's responses to the brand-new Client History Form. By pressing the History button to the right of each field, you can see the response your client submitted to the corresponding question on the Client History Form and pull their response into the field. Alternatively, pressing the History button at the top of the Biopsychosocial Assessment section will allow you to pull forward the client's response to all questions at once.
Plan
We realize that not every assessment can be covered in a single session, yet many third-party payers or regulatory bodies require a treatment plan to be completed immediately after the first session. The new Plan field allows you to document a simple plan for moving forward such as continuing your assessment, requesting records from other providers, or coordinating care with a primary care doctor without utilizing the full treatment plan template. This field is optional.
Psychotherapy Progress Notes
Based on industry research and customer feedback we've made some important and exciting changes to the Psychotherapy Progress Note.
Current Mental Status
The Patient Presentation section has been replaced with the improved Current Mental Status. This is the same section that appears on Psychotherapy Intake Notes. All of these fields are optional. We kept the one-click options to mark the whole section as not assessed and within normal limits, and the History button will now be able to show both Psychotherapy Intake and Psychotherapy Progress Notes in one view.
Risk Assessment
Just like on our Psychotherapy Intake Note, we’ve replaced the Safety Issues section on the Psychotherapy Progress Note with our new Risk Assessment. It will be easier than ever to do a thorough, effective assessment of risks at every session and document that assessment appropriately.
Section Header Updates
TherapyNotes™ note templates have always been based on the SOAP format. We’ve updated the section headers to make it easier to understand what goes in each field.
- Symptom Description and Subjective Report is still where your client’s report of symptoms and relevant experiences, information from collateral contacts, and other subjective data can be documented.
- Relevant Content has been renamed Objective Content to follow the SOAP acronym, but it’s still the place to document content of discussions and your observations of what happened during the session. You will still be able to document interventions with the customizable list in the Interventions Used section, and Treatment Plan Progress will stay the same as well.
- Additional Notes Regarding Goals and Objectives has been renamed to Additional Notes/Assessment to better guide content in this field. You may want to document your assessment of the client’s progress, reactions to interventions, therapeutic processes, or medical necessity for treatment here. You also may have specific documentation requirements from third parties, such as insurance companies or licensing boards, that don’t fit neatly into other sections of the note.
- Additional Notes / Assessment and Plan headers have also been reformatted to be more in line with other section headers.
Psychiatry Notes
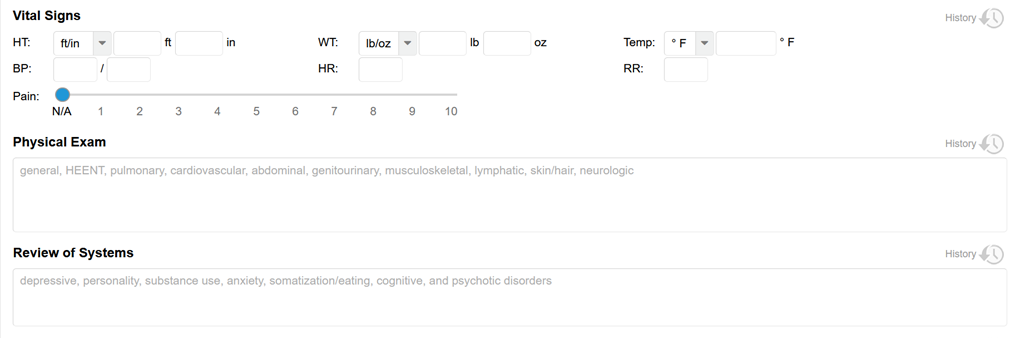
Psychiatry Progress Notes also feature many of these improvements, including updates to the Current Mental Status, Risk Assessment, and Biopsychosocial Assessment sections and the inclusion of the new Vital Signs, Physical Exam, Review of Systems, and Plan fields. Just like our Psychotherapy Note templates, information can flow smoothly from intake to sessions making documentation swift and easy. History functionality is available making it possible to review previous sessions and prepare for your next.
* The content of this post is intended to serve as general advice and information. It is not to be taken as legal advice and may not account for all rules and regulations in every jurisdiction. For legal advice, please contact an attorney.
Get more content like this, delivered right to your inbox. Subscribe to our newsletter.
More Content You'll Enjoy

What’s New: TherapySearch Practice Link, Edit Medications, and NPP Update

Required Updates to Your Notice of Privacy Practices
